LOS ANGELES – California struggled to hospital staff and classrooms as an amazing surge in Coronavirus infection swept the country.
Omicron variants that spread quickly from Covid-19 are health workers exposed or infected even when hospital beds fill with patients and “some facilities will be bound,” Secretary of Health and Human Dr Mark Ghaly said on Wednesday.
About 40% of hospitals expect to face critical staff shortages and some reported as a quarter of their staff for reasons related to the virus, Kiyomi Burchill said from the Association of the California Hospital.
In Fresno County, more than 300 workers in hospital areas are isolated because of exposure or recovery, said and Lynch, director of district emergency medical services.
The Los Angeles County firefighters drove a patient to a hospital in a fire truck rather than an ambulance because 450 firefighters did not exist after testing the positive head assistant Brian Bennett told Carson City Council on Tuesday, according to The Los Angeles Daily News.
In the future, the district fire department will only be sent on medical calls when absolutely necessary, officials said.
“The distribution of fast omicrons has destroyed our workforce,” McCormick Ambulance, a private company contracted with the county, said in a statement.
California has the lowest level per capita case in the US in September but like other countries, now experiences a dramatic increase from the Omicron variant.
The confirmed virus case has surged almost 500% in the past two weeks and hospitalization has doubled since Christmas to more than 8,000.
Inpatient hospitalization countries can reach 20,000 early next month, the level of almost as high as last January, when California experienced the most deadly wave.
At least nine hospitals in Orange County have established a surge wave to increase their capacity if they are flooded by virus cases in addition to the increase in other medical problems, such as strokes, said Dr.
Regina Chinsio-Kwong, Deputy Director of Regional Health.
People with small symptoms must begin with a virtual visit to the doctor because of our hospitals and our ers and our full care is full and they really need to focus their efforts on people who are truly sick, “he said.
California has extended its indoor mask mandate to mid-February to help fight infection but Ghaly said there was no discussion about further restrictions, recorded the availability of vaccines and covid-19 treatment, which were largely not present a year ago.
This virus ruled out school personnel even when 6 million K-12 students returned to the classroom.
Sacramento City Unified School District reported that more than 500 students and staff were quarantined after positive testing for Covid-19.
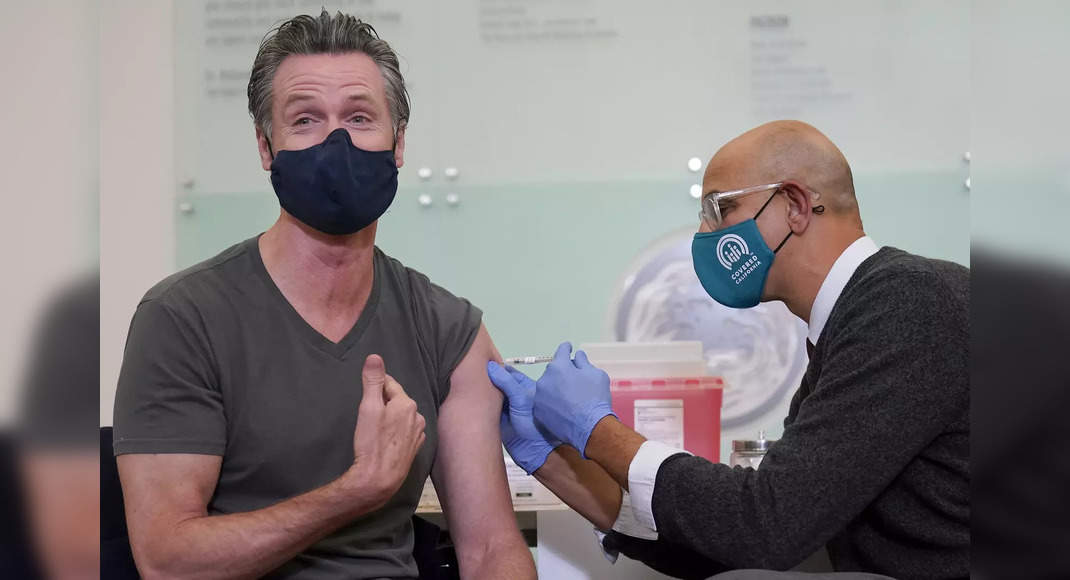
Governor Gavin Newsom and State Officials, meanwhile, faced criticism for failing to fulfill the promise to provide a quick test, at home for all California students and school staff before the classroom reopened after a winter holiday.
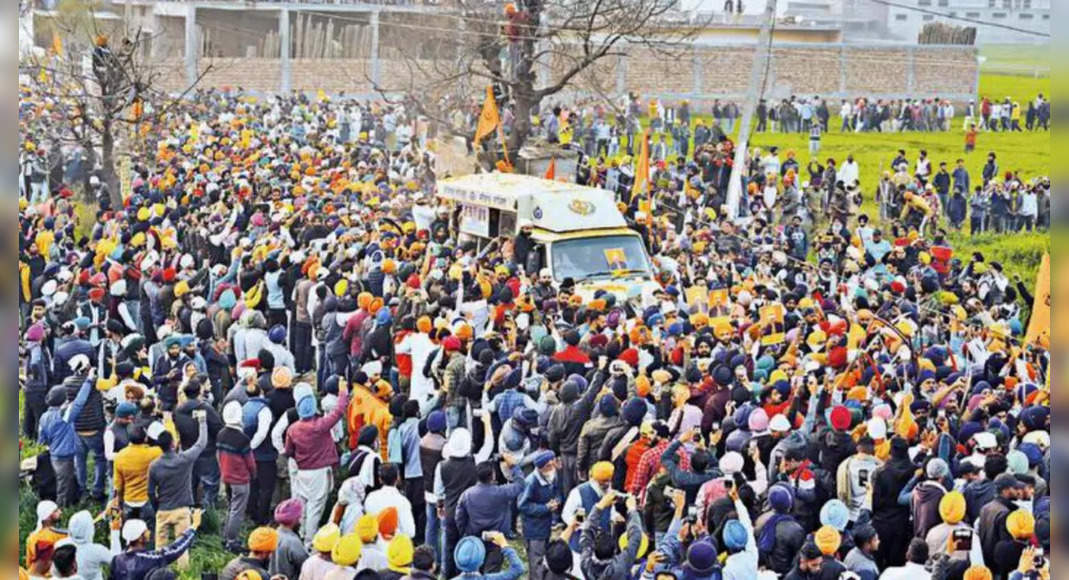
Millions of test kits are sent to family but millions more are not, and there is a long line of this week at the Los Angeles County test site.
The Principal of California Tony Thurmond on Wednesday called the delay “disappointing.” Ghaly said the problem of logistics and bad weather in South California has contributed to the problem but said that around 6.2 million tests have been submitted to local education offices, with more tests out this week.